French national reference center for idiopathic nephrotic syndrome in children and adults (INS)
 The « idiopathic nephrotic syndrome (INS) in children and adults » reference center, whose coordinator is Pr Audard (Henri-Mondor hospital), was created in 2006. It was re-labeled following the evaluation of a jury mandated by the DGOS in 2017 and 2023.
The « idiopathic nephrotic syndrome (INS) in children and adults » reference center, whose coordinator is Pr Audard (Henri-Mondor hospital), was created in 2006. It was re-labeled following the evaluation of a jury mandated by the DGOS in 2017 and 2023.
The reference center is made up of a coordinating center, 4 constituent reference centers and 21 competence centers, thus ensuring the networking of the entire territory.
The INS reference center aims to continue the work initiated more than 15 years ago in the fields of care, expertise, medico-social and therapeutic education.
The Necker constitutent center is particularly involved in the transition from pediatric to adult nephrology, as both services are located on the same site. Joint consultations with pediatric nephrologists and adult nephrologists, as well as frequent joint meetings, help to harmonize therapeutic management and ensure continuity of care when pediatric patients are transferred to adult facilities. Professor Bertrand Knebelmann, in charge of adult nephrology, and Professor Olivia Boyer, in charge of pediatric nephrology, are key players in this collaborative approach aimed at ensuring the well-being and optimum health of patients throughout their medical journey.
This center of reference is affiliated to the ORKID rare diseases healthcare network, the ERKNet European reference network (ERN), and the Transplantchild European reference network (ERN).
Keywords : Idiopathic nephrotic syndrome, Extramembranous glomerulonephritis, Focal and segmental hyalinosis.
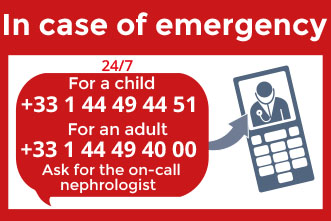
Contact us
For a child*:
Phone. +33 (0)1 44 49 44 67
*Doctolib is reserved for follow-up consultation requests
For a first consultation request, please submit your request via this online form
For professionals : Request a review
For an adult patient :
(1st consultation and follow-up)
Phone. +33 (0)1 44 49 54 16
Idiopathic nephrotic syndrome in children
What is idiopathic nephrotic syndrome in children?
The kidneys contain glomeruli that filter the blood, functioning like « noodle sieves », retaining large substances (proteins and blood cells) and letting through waste products, small substances mostly from food, such as water, salt, urea. These filtered wastes are then found in the urine.
 A nephrotic syndrome occurs when the holes in the sieve of the glomeruli widen, allowing proteins, mainly albumin (albuminuria), to pass into the urine. The result is a decrease in the concentration of albumin in the blood, which normally ensures the maintenance of water and salt in the blood through a « sponge » effect. The water and salt will then pass from the bloodstream to the rest of the body and cause edemas.
A nephrotic syndrome occurs when the holes in the sieve of the glomeruli widen, allowing proteins, mainly albumin (albuminuria), to pass into the urine. The result is a decrease in the concentration of albumin in the blood, which normally ensures the maintenance of water and salt in the blood through a « sponge » effect. The water and salt will then pass from the bloodstream to the rest of the body and cause edemas.
In children, nephrotic syndrome is most often related to what is called idiopathic nephrotic syndrome (the cause of which is not known), also known as nephrosis.
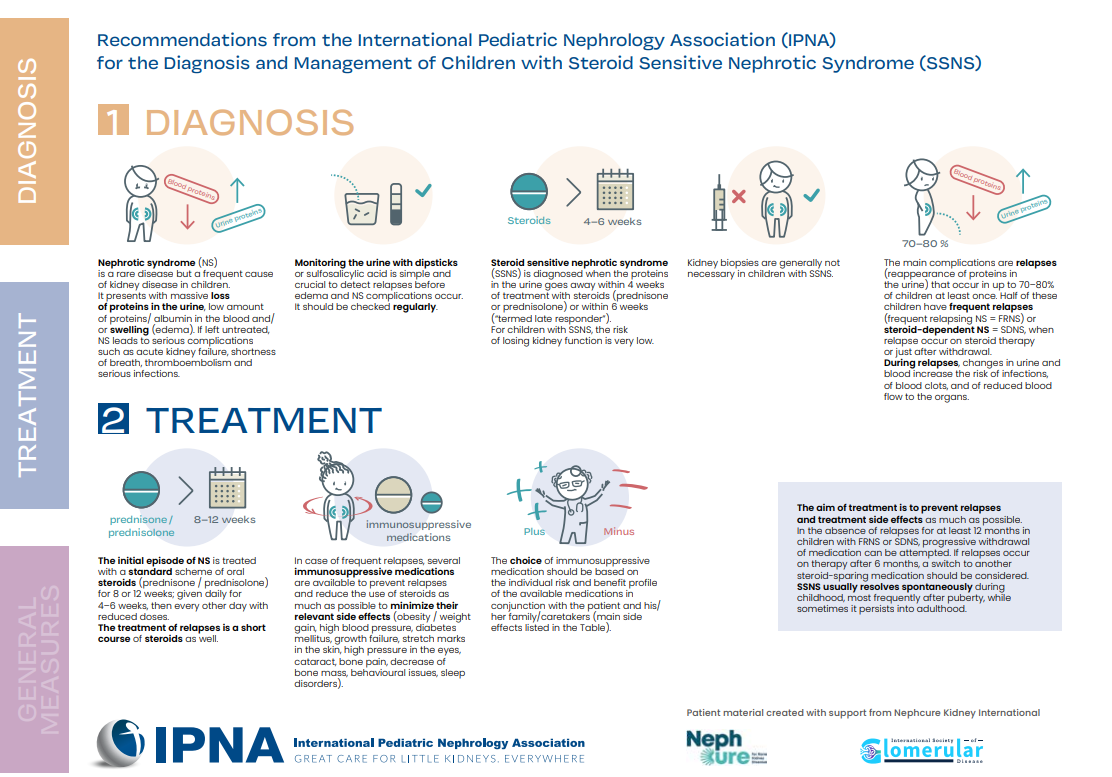
There are two forms of idiopathic nephrotic syndrome based on response to treatment :
- Steroid sensitive nephrotic syndrome when standard treatment with cortisone (prednisone) achieves complete remission, i.e. making the filter impermeable to protein again and making the protein disappear in the urine; and conversely
-
Steroid resistant nephrotic syndrome (See SRNS sheet in French).
Idiopathic nephrotic syndrome « responds » eight times out of ten to cortisone. The disappearance of proteinuria is quickly accompanied by the disappearance of edemas.
How common is idiopathic nephrotic syndrome in the population?
It is a rare disease that affects about 1 to 5 children per 100,000. The disease is more common in boys than in girls.
What are the causes and means of transmission of idiopathic nephrotic syndrome?
Idiopathic nephrotic syndrome is a disease of which the precise cause is not known.
Nephrotic syndromes that are put into remission with immunosuppressive treatment seem to be linked to an abnormality in the cells of the immune system (white blood cells) which would manufacture one or more products circulating in the blood, which would increase the permeability of the glomerular filter to proteins (widening of the holes in the sieve). The cause(s) of this immune dysfunction are currently not identified.
Conversely, about one-third of nephrotic syndromes that do not go into remission with immunosuppressive therapy have a genetic origin most often related to structural abnormalities of certain proteins in podocytes (glomerular filter cells) (see Hereditary SRNS sheet, Congenital NS sheet).
However, all the genetic causes of steroid-resistant nephrotic syndrome are not yet known.
What are the symptoms of idiopathic nephrotic syndrome?
A nephrotic syndrome is suspected when there is edemas, responsible for puffiness of the eyelids in the morning and swelling of the ankles during the day when standing.
Too much water and salt in the body can also cause swelling of the abdomen (ascites), bursa in boys (hydrocele), water accumulation around the lungs (pleural effusion). These edemas are troublesome, but most often they are not dangerous.
Faced with these edemas, it is easy to affirm that it is a nephrotic syndrome by looking for the presence of proteins in the urine.
In other cases, there are no symptoms and the diagnosis is made by chance during a blood or urine test.
Finally, it can be revealed by various complications: abdominal pain, shortness of breath, infection, headaches, clots in the circulation (thrombosis) that can move and cause a clot in the lungs (pulmonary embolism).
What tests should be taken for the diagnosis?
When the diagnosis is suspected, the urine is tested for protein. When the test strip is positive for protein, it is important to specify the amount of protein lost in the urine. This can be done in the laboratory on a morning sample or on a urine collection for 12 or 24 hours.
The diagnosis is then confirmed by a blood test. Many diseases affecting the kidneys can be responsible for edemas and proteins in the urine. For this reason, specialized examinations may be necessary.
Thus, a kidney biopsy may be indicated at the time of diagnosis if there are clinical symptoms or biological findings suggesting that the nephrotic syndrome is related to another disease. It is also indicated in children who still retain protein in the urine after one month of treatment with corticosteroids (See steroid-resistant nephrotic syndrome fact sheets).
Which organs are affected?
Apart from edemas, which are often unsightly but usually without severe consequences (and which leave no traces), the nephrotic syndrome exposes to certain complications.
Infections
- Bacterial infections are common and can occur early in the course of the disease. They may include peritonitis (infection around the intestines) leading to severe abdominal pain and fever, meningitis, pneumonia or cellulitis (infection of the subcutaneous tissues). All of these infections can be controlled with antibiotics.
- Viral infections can also be favored by treatment given to treat nephrotic syndrome, such as prednisone or immunosuppressants. This is particularly the case with chickenpox which can be serious. There are effective medicines that should be given if chickenpox occurs to prevent complications of the disease, and if you come into contact with someone with chickenpox to prevent its occurrence.
Thromboses
Nephrotic syndrome is responsible for coagulation abnormalities that increase the risk of blood clots forming in the circulation. These are thrombosis accidents that can be localized in the veins of the arms or legs, renal veins, brain vessels, pulmonary arteries. These accidents can be prevented by taking medicines called anticoagulants (which thin the blood).
Other complications
When the treatments are not effective and do not lead to remission (complete disappearance of proteins in the urine), urine protein leakage can be responsible, in the long term, for a state of malnutrition with muscle wasting, height growth disorders, disturbances in lipid profile and thyroid dysfunction. Scars may appear and progress in the kidneys, leading to chronic kidney failure within an unspecified period of time, which may be several years.
What are the treatments to follow?
The treatment has two goals :
limit the consequences of the nephrotic syndrome, in particular edemas, and make proteinuria disappear.
Edemas are the consequence of a decrease in the elimination of salt by the kidneys. The diet should therefore be as low in salt as possible. Salt-rich foods should be avoided and no salt should be added to food at mealtimes. Diuretics, drugs that increase salt elimination by the kidneys, should be used with caution as they can promote the formation of clots in the bloodstream. Albumin infusions are rarely necessary.
In order to regress proteinuria, treatment is based on corticosteroid therapy: prednisone (Cortancyl®) or a drug of the same family, such as prednisolone (Solupred®). It is associated with a diet limited in salt, sugars and fats, and a supplementation of calcium and vitamin D (see below).
If proteinuria persists after one month, three infusions of high doses of corticosteroids (prednisone equivalent, administered intravenously) are given, each 48 hours apart. If the proteinuria persists one week after the infusions, the nephrotic syndrome is said to be “steroid-resistant”. (see sheets in French)
Two in three children with steroid-sensitive nephrotic syndrome will have one or more relapses when the dose of prednisone is lowered or after stopping treatment. They are often favored by an infection such as nasopharyngitis or angina. Recovery, either spontaneously or by antibiotic therapy, of the infectious episode can lead to remission.
It is sometimes suggested that corticosteroid therapy be given daily during infections to prevent relapse. An allergy can also be a factor in relapse. Relapse treatment consists of increasing the corticosteroid therapy, which is given daily until remission is achieved, then given again every other day at a decreasing dose.
If the dose of prednisone necessary to maintain remission is too high causing a risk of significant side effects, the use of other immunosuppressive treatments (i.e. based on molecules that limit the action of white blood cells) is necessary. These are in particular levamisole (Elmisol®), mycophenolate mofetil (Cellcept®), cyclosporine (Neoral®) and tacrolimus (Prograf®), cyclophosphamide (Endoxan®), rituximab (Mabthéra®). Other treatments being evaluated may be offered.
There is no treatment allowing a total cure in all patients at this time.
What are the side effects of steroids?
Steroids and other drugs used have potential side effects.
The side effects of prednisone treatment depend on the dose the child receives, but also vary from child to child for the same dose, with some children more likely to develop a complication than others. As the dose decreases, especially when the treatment is given every other day, the side effects also decrease.
Possible side effects include :
- Change in physical appearance :
Red cheeks, increased hairiness. The skin is more fragile. Teens can develop stretch marks and acne, for which the advice of a dermatologist is helpful.
- Appetite stimulation :
Corticosteroid therapy can cause rapid and unbalanced weight gain, with big cheeks and a big belly. A diet low in sugar and fat must be followed to avoid excessive weight gain. Eating outside of mealtimes should be avoided. Reducing sugar consumption is recommended: elimination of rapidly absorbed sugars, sweets, cakes, chocolate, jams and sweetened drinks. Avoiding high-fat foods by reducing butter and cheese is also recommended.
- Character disorders :
Children receiving prednisone are often very active, restless. They may have temper tantrums and trouble sleeping. Some children are sadder. They may be aggressive when they used to be very calm children. These problems disappear when the doses of prednisone are reduced.
- Increase in blood pressure :
This is why the diet should be low in salt even when the proteinuria has subsided. It is only when the steroid dose is low that salt intake can be increased.
- Height growth disorders :
Steroids, especially in high doses and given daily, block growth. It restarts when the doses are decreased and especially when the treatment is given every other day. If the doses needed to keep the child in remission are too high and are responsible for slowing growth, the doctor may decide to introduce another treatment.
- Less resistance to infections :
Treatment with prednisone decreases the immune system. In case of fever, a doctor should be consulted promptly.
- Bone problems :
Steroid treatment can be responsible for calcium loss in the bones (osteoporosis), which is why a calcium and vitamin D supplement is often prescribed. Disorders of the vascularization of certain areas of the bones (osteonecrosis) may occur and result in pain. Immobilization in a cast may then be necessary.
- Eye problems :
Prolonged treatment can cause a cataract, which can be detected by an ophthalmologic examination before it leads to blurred vision.
- Problems when stopping treatment :
After prolonged treatment, its abrupt cessation can have serious consequences because the body no longer produces enough cortisol, the natural equivalent of prednisone. In these cases, hydrocortisone replacement therapy may be necessary for a few weeks.
How does steroid sensitive nephrotic syndrome progress in the long term, in adulthood?
The disease may last longer if the nephrotic syndrome started early in childhood, before 4 to 5 years old.
However, the number of relapses each year tends to decrease over time. It is impossible to predict how long the illness will last. There is definitely a risk that the disease will continue to relapse into adulthood. About 40% of people who had multiple relapses in childhood continue to have relapses into adulthood.
As long as the nephrotic syndrome continues to respond to treatment, which is most often the case, there is virtually no risk of the disease becoming complicated by chronic kidney failure.
How is idiopathic nephrotic syndrome in children monitored?
At home, the child and his parents should test daily or every two to three days for proteins in the urine (proteinuria).
The simplest way to do this is to use strips, such as Albustix®, which are dipped in urine and then compared with the color of the strips indicated on the bottle. The color of the strip will change from yellow when there is no proteinuria to light or dark green depending on the degree of proteinuria.
We can thus know if this search for proteinuria is negative or positive, with a scale of one, two, three or four crosses. The presence of « traces » should not be a cause for concern. The results are noted in a follow-up booklet.
When the protein test strip is positive, it is important to specify the amount of protein lost in the urine. This can be done in the laboratory on a urine collection.
The advantage of regular urine monitoring with the Albustix® strip is that it can detect a relapse long before edemas occur. Treatment is then started quickly to limit the consequences of this relapse. In addition, remission is achieved more quickly if the relapse is treated without delay.
In addition to regular monitoring of proteinuria and blood albumin levels, the doctor regularly checks growth, kidney function (urea and blood and urine creatinine), and immunosuppressive drug dosages.
Monitoring also concerns the child’s weight, which may increase in case of edemas or due to steroid therapy which stimulates the appetite.
Steroid resistant nephrotic syndrome
What is steroid resistant nephrotic syndrome?
The kidneys allow, thanks to glomeruli, a kind of filter or « waste sorting plant », to eliminate certain components present in the blood and coming mainly from food, such as water, salt, urea from proteins present in meat or dairy products. This filter is very selective and does not let through certain substances such as proteins produced by the body.
A nephrotic syndrome occurs when this filter is too permeable and the kidneys allow large amounts of protein, especially albumin, present in the bloodstream to pass through the urine. The result is a decrease in the concentration of albumin in the blood and a difficulty for the kidneys to eliminate salt and water from the diet. Water and salt will pass from the bloodstream into the tissues and cause edemas.
Nephrotic syndrome is said to be steroid resistant when the standard treatment of nephrotic syndrome with cortisone (prednisone) does not achieve complete remission, i.e. to make the filter impermeable again to proteins and to remove the proteins in the urine.
How common is steroid resistant nephrotic syndrome in the population?
The exact number of new cases annually in the general population is unknown. All nephrotic syndromes affect 1 to 4 in 100,000 children, and 5 to 10% of them are steroid resistant.
What are the causes and means of transmission of the steroid resistant nephrotic syndrome?
Sporadic steroid resistant idiopathic nephrotic syndrome is a heterogeneous disease. Approximately one third has a genetic origin most often related to structural abnormalities of certain proteins in podocytes (cells of the glomerular filter). (see https://www.filiereorkid.com/la-fonction-renale/). All the genetic causes of steroid resistant nephrotic syndrome are not yet known.
The others have a totally different and yet unsolved mechanism. One of the hypotheses put forward is that the cells of the immune system produce one or more circulating factors that increase the permeability of the glomerular filter to proteins.
Current research focuses on the search for new genes and the identification of circulating factors responsible for nephrotic syndrome.
What are the symptoms of steroid resistant nephrotic syndrome?
A nephrotic syndrome is suspected when there are edemas, responsible for puffiness of the eyelids in the morning, swelling of the ankles during the day when standing. Excess water and salt in the body can also cause swelling of the abdomen (ascites), bursae in boys (hydrocoele), an effusion in the pleura surrounding the lungs (pleural effusion). These edemas are bothersome, but most often are not dangerous.
Faced with these edemas, one can easily affirm that it is a nephrotic syndrome by looking for the presence of proteins in the urine.
In other cases, there are no symptoms and the diagnosis is made incidentally during a blood or urine test.
Finally, it can be revealed by various complications: abdominal pain, shortness of breath, infection, headaches, clots in the circulation (thrombosis) that can move and lead to a pulmonary embolism.
What tests must be taken for the diagnosis?
When the diagnosis is suspected, we look for proteins in the urine. The simplest way to do this is to use strips, such as Albustix®, which are dipped into the urine and then compared in color with those on the vial. The color of the strip will change from yellow when there is no proteinuria to light or dark green depending on the degree of proteinuria. This will indicate whether the proteinuria test is negative or positive on a scale of one, two, three or four crosses. The presence of « traces » should not be a cause for concern.
When the protein test strip is positive, it is important to specify the amount of protein lost in the urine. This can be done in the laboratory on a morning sample or on a 12-hour or 24-hour urine collection.
The diagnosis is then confirmed by a blood test, usually followed by a kidney biopsy, and a genetic analysis that takes several months. All the genetic causes of steroid resistant nephrotic syndrome are not yet known.
What are the treatments to follow?
The treatment has two goals: to make the proteinuria disappear and to limit the consequences of the nephrotic syndrome, in particular edemas.
In order to regress proteinuria, immunosuppressive treatments, particularly cyclosporine and tacrolimus, can have a beneficial effect in combination with steroids (prednisone). Other treatments are currently being evaluated and may be proposed.
If necessary, treatment to prevent complications of nephrotic syndrome is associated with it. To reduce swelling, a salt-free diet, regular albumin infusions and diuretics are prescribed. Treatments to reduce proteinuria and protect the kidney, anticoagulants to limit the risk of thrombosis, treatments to reduce cholesterol and triglyceride levels and/or synthetic thyroid hormones and/or synthetic growth hormone are also prescribed. Nevertheless, progression to end-stage renal disease is frequent and requires dialysis and/or a kidney transplant. In this case, there is a risk of recurrence of nephrotic syndrome after kidney transplantation.
Which organs are affected?
Apart from edemas, often unsightly but usually without severe consequences, nephrotic syndrome exposes to certain complications.
- Infections : Bacterial infections are common and can occur early in the course of the disease. They may include peritonitis (infection of the peritoneum) causing severe abdominal pain and fever, meningitis, pneumonia or cellulitis (infection of the subcutaneous tissues). All of these infections can be controlled with antibiotics. Viral infections may be promoted by the treatment given to treat nephrotic syndrome such as prednisone or immunosuppressants. This is particularly the case with chickenpox, which can be serious. There are effective medications that should be given if chickenpox develops to avoid complications of the disease, and if contact is made with a person who has chickenpox to prevent its onset.
- Thrombosis: Nephrotic syndrome is responsible for coagulation abnormalities that increase the risk of blood clots forming in the circulation. These are thrombosis events that can be localized in the veins of the upper or lower limbs, renal veins, cerebral vessels, pulmonary arteries. The clots can move and cause a pulmonary embolism. These accidents can be prevented by taking medication called anticoagulants.
- Other complications : When treatments are not effective and do not lead to remission, urinary leakage of protein can be responsible, in the long term, for a state of malnutrition with muscle wasting, Height growth disorder, disturbances in lipid profile and thyroid insufficiency. Sclerosis lesions may appear and progress in the kidneys, leading to chronic kidney failure within an unspecified period of time, which may be several years.
Certain very rare genetic forms are associated with damage to other organs (heart, eye, nervous system, etc.).
How is steroid resistant nephrotic syndrome monitored?
In addition to regular monitoring of proteinuria and blood albumin levels, growth, kidney function (urea and blood and urinary creatinine), and immunosuppressive drug dosages are monitored regularly.
Membranous glomerulonephritis
What is membranous glomerulonephritis?
The kidneys contain glomeruli that filter the blood, functioning like sieves, retaining large substances (proteins and blood cells) and letting through waste products, small substances mainly from food, such as water, salt, urea. These filtered wastes are then found in the urine.
 A nephrotic syndrome occurs when the holes in the sieve widen, allowing proteins (proteinuria), mainly albumin, to pass into the urine (albuminuria). The result is a decrease in the concentration of albumin in the blood, which normally ensures the maintenance of water and salt in the blood through a « sponge » effect. The water and salt will therefore pass from the bloodstream into the tissues and cause edemas.
A nephrotic syndrome occurs when the holes in the sieve widen, allowing proteins (proteinuria), mainly albumin, to pass into the urine (albuminuria). The result is a decrease in the concentration of albumin in the blood, which normally ensures the maintenance of water and salt in the blood through a « sponge » effect. The water and salt will therefore pass from the bloodstream into the tissues and cause edemas.
Membranous glomerulonephritis (MGN) is the most common cause of nephrotic syndrome in adults over the age of 50. It is characterized by granular deposits of antibodies on the outer side of the filter on kidney biopsy, which explains the term « membranous ».
How common is membranous glomerulonephritis?
The exact number of new cases annually in the general population remains poorly known. It is estimated at 1.3 per 100,000 adults. It is therefore a rare disease.
What is the evolution of membranous glomerulonephritis?
The evolution is highly variable from one patient to another: approximately one third of patients go into spontaneous remission, one third remain with variable proteinuria and may have some degree of renal failure, and one third progress to severe chronic renal failure requiring dialysis or transplantation. The disease can recur on the graft after kidney transplantation in almost 50% of cases and eventually compromise its function.
What causes membranous glomerulonephritis?
MGN is sometimes associated with another disease such as cancer, infections, especially viral (hepatitis B) or parasitic infections, or the use of certain drugs. Most often, it occurs without any other apparent disease, justifying until recently the term idiopathic.
 MGN is an autoimmune disease, characterized by the production of antibodies directed against our own antigens located in the glomerular filters.
MGN is an autoimmune disease, characterized by the production of antibodies directed against our own antigens located in the glomerular filters.
The Parisian team at the Tenon Hospital was the first to identify such an antigen in newborn children (1), and contributed with the Nice team to identify antigens in adults using different techniques, based on genetics or biochemistry. These antigens have code names whose meaning is of little importance, whether they are NEP in children or adults, PLA2R1 in about 80% of cases (2), or THSD7A (3) in less than 5% of cases. Thus, there are still other antigens to be discovered.
Our immune system normally produces antibodies to protect us against the various pathogens in our environment (bacteria, viruses, parasites…). For as yet unknown reasons, within the framework of GEMs, our organism produces antibodies against proteins (PLA2R1, THSD7A) which form the meshes of this sieve.
There are also cases in children that are due to the production of antibodies against food antigens such as beef albumin brought by meat or milk (4), which brings to mind the increasingly important role of the environment, including pollution.
What are the symptoms of membranous glomerulonephritis?
A nephrotic syndrome is suspected when there are edemas, responsible for puffiness of the eyelids in the morning and swelling of the ankles during the day. Excess water and salt in the body can also cause an effusion in the envelope (pleura) surrounding the lungs (pleural effusion), and more rarely a swelling of the abdomen (ascites) or the bursae in men (hydrocoele). These edemas are bothersome, but most often, they are not dangerous.
They can be easily linked to nephrotic syndrome by testing for proteins in the urine using a simple test strip.
Sometimes there are no symptoms and the diagnosis is made incidentally during a blood or urine test that reveals proteinuria.
Finally, the disease can be revealed by various complications: abdominal pain, shortness of breath, infection, headaches, clots in the circulation (thrombosis) that can move and rarely lead to a pulmonary embolism.
What tests are required for diagnosis?
When the diagnosis is suspected, we look for proteins in the urine. The simplest way to do this is to use strips, such as Albustix®, which are dipped into the urine and then compared in color with those on the vial. The color of the strip will change from yellow when there is no proteinuria to light or dark green depending on the degree of proteinuria. It can then be determined whether the proteinuria test is negative or positive, with a scale of one, two, three or four crosses. The presence of « traces » should not be a cause for concern.
When the protein test strip is positive, it is important to specify the amount of protein lost in the urine. This can be done in the laboratory on a morning sample or on a 12-hour or 24-hour urine collection.
The diagnosis is then confirmed by a blood test, looking in particular for antibodies specific to the disease (anti-PLA2R1 and anti-THSD7A in adults). A kidney biopsy remains desirable in most patients because it provides additional diagnostic information.
What are the treatments to follow?
The treatment has two goals :
- Symptomatic, i.e. it addresses the symptoms (decrease proteinuria and edemas) and aims to prevent complications of the disease,
- Curative, healing the patient, preventing the production of antibodies.
Since one third of patients go into remission spontaneously, treatment is often initially symptomatic for 6 months in the absence of signs of severity (progressive renal failure or serious complications of nephrotic syndrome). A treatment that blocks the renin-angiotensin-aldosterone system (conversion enzyme inhibitor or angiotensin II receptor blocker) can reduce proteinuria at the cost of lower blood pressure. It is combined with a salt-free diet and diuretics to reduce edemas. In some cases (very low albumin levels in the blood), anticoagulants to limit the risk of thrombosis and cholesterol-lowering treatments (statins) are also proposed.
The curative treatment of MGN remains controversial. It is based on the use of immunosuppressive drugs (drugs that lower the immune system’s defenses to decrease the production of antibodies). Corticosteroids alone are generally ineffective, and do not achieve complete remission, i.e. making the filter impermeable to proteins again and making proteinuria disappear.
Immunosuppressive therapy is recommended in cases of deterioration of renal function or nephrotic syndrome persisting 6 months after initiation of symptomatic treatment. However, this delay may induce irreversible damage. Until recently, no marker could predict the evolution of a patient. The discovery of anti-PLA2R1 and anti-THSD7A antibodies has led to the identification of new markers predictive of the evolution of renal function. A high level of anti-PLA2R1 antibodies at diagnosis appears to be associated with a lower chance of remission. More important than a high level of antibodies at diagnosis is their persistence in the weeks or months following diagnosis (5). Anti-PLA2R1 antibodies are directed against at least 3 different domains of PLA2R1. It appears that patients immunized against a single PLA2R1 domain go into spontaneous remission more often, whereas patients immunized against multiple PLA2R1 domains appear to have an unfavorable course in the absence of curative treatment with a higher risk of adverse disease progression (6,7). Antibody assays and perhaps analysis of their specificity with respect to the mentioned domains should allow us to propose a more personalized care.
 Nevertheless, progression to severe renal failure is possible, requiring then dialysis and/or a kidney transplant. In this case, there is a risk of MGN recurrence after kidney transplantation (8,9).
Nevertheless, progression to severe renal failure is possible, requiring then dialysis and/or a kidney transplant. In this case, there is a risk of MGN recurrence after kidney transplantation (8,9).
How is membranous glomerulonephritis monitored?
In addition to regular monitoring of proteinuria and blood albumin levels, kidney function (urea and blood creatinine), and anti-PLA2R1 (or more rarely anti-THSD7A) antibody levels are monitored regularly. Measurement of PLA2R1 antibody levels is available in most hospital centers in France. The Nice and Paris-Tenon centers can also perform serum anti-THSD7A antibody testing.
The Nice center has developed techniques for assaying antibodies directed against certain areas of the molecule (epitopes), which for the moment are research techniques, and whose usefulness in the clinic must be validated and demonstrated to be superior to that of simple antibody assays.
Bibliographical references
1. Debiec H, Guigonis V, Mougenot B, Decobert F, Haymann JP, Bensman A, et al. Antenatal membranous glomerulonephritis due to anti-neutral endopeptidase antibodies. N Engl J Med. 2002;346(26):2053-60.
2. Beck LH, Jr., Bonegio RG, Lambeau G, Beck DM, Powell DW, Cummins TD, et al. M-type phospholipase A2 receptor as target antigen in idiopathic membranous nephropathy. N Engl J Med. 2009;361(1):11-21.
3. Tomas NM, Beck LH, Jr., Meyer-Schwesinger C, Seitz-Polski B, Ma H, Zahner G, et al. Thrombospondin type-1 domain-containing 7A in idiopathic membranous nephropathy. N Engl J Med. 2014;371(24):2277-87.
4. Debiec H, Lefeu F, Kemper MJ, Niaudet P, Deschenes G, Remuzzi G, et al. Early-childhood membranous nephropathy due to cationic bovine serum albumin. N Engl J Med. 2011;364(22):2101-10.
5. Dahan K, Debiec H, Plaisier E, Cachanado M, Rousseau A, Wakselman L, Michel PA, Mihout F, Dussol B, Matignon M, Mousson C, Simon T, Ronco P; GEMRITUX Study Group. Rituximab for Severe Membranous Nephropathy: A 6-Month Trial with Extended Follow-Up. J Am Soc Nephrol. 2017 Jan;28(1):348-358.
6. Seitz-Polski B, Dolla G, Payre C, Girard CA, Polidori J, Zorzi K, et al. Epitope Spreading of Autoantibody Response to PLA2R Associates with Poor Prognosis in Membranous Nephropathy. J Am Soc Nephrol. 2016;27(5):1517-33.
7. Seitz-Polski B, Debiec H, Rousseau A, Dahan K, Zaghrini C, Payré C, Esnault VLM, Lambeau G, Ronco P. Phospholipase A2 Receptor 1 Epitope Spreading at Baseline Predicts Reduced Likelihood of Remission of Membranous Nephropathy. J Am Soc Nephrol. 2017 Nov 7. pii: ASN.2017070734. doi: 10.1681/ASN.2017070734.
8. Debiec H, Martin L, Jouanneau C, Dautin G, Mesnard L, Rondeau E, et al. Autoantibodies specific for the phospholipase A2 receptor in recurrent and De Novo membranous nephropathy. Am J Transplant. 2011;11(10):2144-52.
9. Seitz-Polski B, Payre C, Ambrosetti D, Albano L, Cassuto-Viguier E, Berguignat M, et al. Prediction of membranous nephropathy recurrence after transplantation by monitoring of anti-PLA2R1 (M-type phospholipase A2 receptor) autoantibodies: a case series of 15 patients. Nephrol Dial Transplant. 2014;29(12):2334-42.
Other pathologies
- Post-transplant recurrence of idiopathic nephrotic syndrome
- Idiopathic nephrotic syndrome with minimal steroid sensitive glomerular lesions in adults
Pediatric nephrology
Pediatric nephrologist
Pr Olivia Gillion-Boyer
MD, PhD
Pediatric nephrologist
Dr Laurence Heidet
MD, PhD

Pediatric nephrologist
Dr Marina Charbit
MD, PhD

Pediatric nephrologist
Pr Rémi Salomon
MD, PhD

Pediatric nephologist
Dr Nathalie Biebuyck-Gouge
MD

Pediatric nephrologist
Dr Laurène Dehoux
MD
Adult nephrology
Adult nephrologist
Pr Bertrand Knebelmann
MD, PhD

Adult nephrologist
Dr Aude Servais
MD, PhD
Research
Research for new genes involved in hereditary nephrotic syndromes
Research of new therapeutic strategies in hereditary nephrotic syndromes
- LYMPHOSNIT : Biomarker Research in Idiopathic Nephrotic Syndrome ANSM Association Funding
- GLUCOPED : Study of corticosteroid pharmacokinetics in children (NCT02252237)
- NEPHROVIR-3: Randomized trial investigating the value of elmisole in the first relapse of steroid-sensitive idiopathic nephrotic syndrome
- NEPHRITUX STUDY ORPHA276778: A prospective randomised double blind placebo-controlled phase II/II study evaluating the efficacy of Rituximab in the prevention of relapse of calcineurin dependent idiopathic nephrotic syndrome of childhood-FR (National study)
- RITUXIVIG : Efficacy and safety of immunoglobulin associated with Rituximab versus Rituximab alone in childhood-onset steroid-dependent nephrotic syndrome (RITUXIVIG)
- RIFIREINS : Rituximab from the first episode of minimal change nephrotic syndrome for preventing relapse risk in adult patients: a multicenter randomized controlled trial
- INS Biobank: From immune system damage to podocyte cell damage: prospective database and biological collection of patients (children and adults) suffering from minimal change disease (MCD) and primary focal segmental glomerulosclerosis (FSGS).
- PMNN: « Customized care of membranous glomerulonephritis » – PMMN
Education
IUD Pediatric nephrology
Paris university

2021
– Steroid Avoidance in Low-Immunologic Risk Kidney Transplant Recipients: The New Normal?
Christophe Legendre
Kidney Int Rep, 2021 Dec 16, PMID: 35155852 PMCID: PMC8821038 DOI: 10.1016/j.ekir.2021.12.016
– CRISPR/Cas9-Engineered HLA-Deleted Glomerular Endothelial Cells as a Tool to Predict Pathogenic Non-HLA Antibodies in Kidney Transplant Recipients.
Baptiste Lamarthée, Carole Burger, Charlotte Leclaire, Emilie Lebraud, Aniela Zablocki, Lise Morin, Xavier Lebreton, Béatrice Charreau, Renaud Snanoudj, Soëli Charbonnier, Tifanie Blein, Mélanie Hardy, Julien Zuber, Simon Satchell, Morgan Gallazzini, Fabiola Terzi, Christophe Legendre, Jean Luc Taupin, Marion Rabant, Claire Tinel, Dany Anglicheau
J Am Soc Nephrol, 2021 Dec, PMID: 35167486 PMCID: PMC8638404 DOI: 10.1681/ASN.2021050689
– Weak antibody response to three doses of mRNA vaccine in kidney transplant recipients treated with belatacept.
Nathalie Chavarot, Antoine Morel, Marianne Leruez-Ville, Estelle Vilain, Gillian Divard, Carole Burger, Alexandra Serris, Rebecca Sberro-Soussan, Frank Martinez, Lucile Amrouche, Lynda Bererhi, Fanny Lanternier, Christophe Legendre, Julien Zuber, Dany Anglicheau, Anne Scemla
Am J Transplant, 2021 Dec, PMID: 34431207 PMCID: PMC9906354 DOI: 10.1111/ajt.16814
– Therapeutic plasma exchange for life-threatening pediatric disorders.
Jean-Sébastien Diana, Sandra Manceau, Tioka Rabeony, Caroline Elie, Valérie Jolaine, Sandrine Zamora, Mélodie Aubart, Nadège Salvi, Christine Bodemer, Brigitte Bader-Meunier, Christine Barnerias, Franck Iserin, Christophe Chardot, Florence Lacaille, Sylvain Renolleau, Rémi Salomon, Laure Joseph, Marina Cavazzana, François Lefrère, Laurent Dupic, Marianne Delville
J Clin Apher, 2021 Dec, PMID: 34469617 DOI: 10.1002/jca.21934
– Management of post-transplant recurrent focal and segmental glomerulosclerosis.
Gabriel Morin, Christophe Legendre, Guillaume Canaud
Nephrol Dial Transplant, 2021 Nov 9, PMID: 32087022 DOI: 10.1093/ndt/gfaa021
– Glomerular endothelial cell senescence drives age-related kidney disease through PAI-1.
Camille Cohen, Océane Le Goff, Frédéric Soysouvanh, Florence Vasseur, Marine Tanou, Clément Nguyen, Lucile Amrouche, Julien Le Guen, Oriana Saltel-Fulero, Tanguy Meunier, Thao Nguyen-Khoa, Marion Rabant, Dominique Nochy, Christophe Legendre, Gérard Friedlander, Bennett G Childs, Daren J Baker, Bertrand Knebelmann, Dany Anglicheau, Fabien Milliat, Fabiola Terzi
EMBO Mol Med, 2021 Nov 8, PMID: 34725920 PMCID: PMC8573606 DOI: 10.15252/emmm.202114146
– External validation of a predictive model to estimate renal function after living donor nephrectomy.
Thibaut Benoit, Thomas Prudhomme, Aurélien Adypagavane, Bernard Malavaud, Michel Soulié, Xavier Gamé, Nassim Kamar, Charles Dariane, Christophe Legendre, Arnaud Méjean, Mathieu Roumiguié, Marc Olivier Timsit
Transplantation, 2021 Nov 1, PMID: 33496555 DOI: 10.1097/TP.0000000000003643
– Neurological involvement in monogenic podocytopathies.
Olivia Boyer, Géraldine Mollet, Guillaume Dorval
Pediatr Nephrol, 2021 Nov, PMID: 33791874 DOI: 10.1007/s00467-020-04903-x
– Clinical Utility of Biochemical Markers for the Prediction of COVID-19-Related Mortality in Kidney Transplant Recipients.
Sophie Caillard, Nathalie Chavarot, Hélène Francois, Marie Matignon, Renaud Snanoudj, Jérôme Tourret, Clarisse Greze, Olivier Thaunat, Luc Frimat, Pierre François Westeel, Philippe Gatault, Christophe Masset, Gilles Blancho, Tristan Legris, Valérie Moal, Nassim Kamar, Mariam Jdidou, Charlotte Colosio, Christiane Mousson, Valentin Goutadier, Antoine Sicard, Dominique Bertrand, Jamal Bamoulid, Paolo Malvezzi, Lionel Couzi, Jonathan M Chemouny, Agnès Duveau, Christophe Mariat, Jean-Philippe Rerolle, Antoine Thierry, Nicolas Bouvier, Dany Anglicheau, Yannick Le Meur, Marc Hazzan; French SOT COVID Registry
Kidney Int Rep, 2021 Oct, PMID: 34254049 PMCID: PMC8264524 DOI: 10.1016/j.ekir.2021.06.034
– A very uncommon cause of acute kidney injury in infancy.
Guillaume Dorval, Estelle Balducci, Sophie Kaltenbach, Maryline Chomton, Saoussen Krid, Marion Rabant, Florence Porcheret, Jean-Paul Duong Van Huyen, Philippe Eckart, Guillaume Mortamet, Christophe Delacourt, Laure de Saint-Blanquat, Laurene Dehoux, Capucine Picard, Rémi Salomon, Bénédicte Neven, Olivia Boyer
Kidney Int, 2021 Oct, PMID: 34556303 DOI: 10.1016/j.kint.2021.06.024
– Rituximab for recurrence of primary focal segmental glomerulosclerosis after kidney transplantation: Results of a nationwide study.
Camille Lanaret, Dany Anglicheau, Vincent Audard, Mathias Büchler, Sophie Caillard, Lionel Couzi, Paolo Malvezzi, Laurent Mesnard, Dominique Bertrand, Franck Martinez, Vincent Pernin, Didier Ducloux, Coralie Poulain, Antoine Thierry, Arnaud Del Bello, Jean P Rerolle, Clarisse Greze, Charlotte Uro-Coste, Julien Aniort, Céline Lambert, Nicolas Bouvier, Betoul Schvartz, Nicolas Maillard, Johnny Sayegh, Julie Oniszczuk, Marie-Pascale Morin, Christophe Legendre, Nassim Kamar, Anne E Heng, Cyril Garrouste
Am J Transplant, 2021 Sep, PMID: 33512779 DOI: 10.1111/ajt.16504
-The genetics of steroid-resistant nephrotic syndrome in adults.
Olivia Boyer, Guillaume Dorval, Aude Servais
Nephrol Dial Transplant, 2021 Aug 27, PMID: 32040156 DOI: 10.1093/ndt/gfz257
– Cannabinoid receptor 1 inhibition in chronic kidney disease: A new therapeutic toolbox.
Myriam Dao, Helene François
Front Endocrinol (Lausanne), 2021 Jul, PMID: 34305821 PMCID: PMC8293381 DOI: 10.3389/fendo.2021.720734
– The case | Membranous nephropathy after alemtuzumab treatment.
Marion Rabant, Kathleen Dessaix, David Buob, Ombeline Fagniez, Oana Ramayana Ailioaie, Catherine Johanet, Christophe Legendre, Mohamad Zaidan
Kidney Int, 2021 Jul, PMID: 34154717 DOI: 10.1016/j.kint.2021.02.030
– The European Rare Kidney Disease Registry (ERKReg): Objectives, design and initial results.
Giulia Bassanese, Tanja Wlodkowski, Aude Servais, Laurence Heidet, Dario Roccatello, Francesco Emma, Elena Levtchenko, Gema Ariceta, Justine Bacchetta, Giovambattista Capasso, Augustina Jankauskiene, Marius Miglinas, Pietro Manuel Ferraro, Giovanni Montini, Jun Oh, Stephane Decramer, Tanja Kersnik Levart, Jack Wetzels, Elisabeth Cornelissen, Olivier Devuyst, Aleksandra Zurowska, Lars Pape, Anja Buescher, Dieter Haffner, Natasa Marcun Varda, Gian Marco Ghiggeri, Giuseppe Remuzzi, Martin Konrad, Germana Longo, Detlef Bockenhauer, Atif Awan, Ilze Andersone, Jaap W Groothoff, Franz Schaefer
Orphanet J Rare Dis, 2021 Jun 2, PMID: 34078418 PMCID: PMC8173879 DOI: 10.1186/s13023-021-01872-8
– Apheresis in adult with refractory idiopathic nephrotic syndrome on native kidneys.
Léa Moret, Alexandre Ganea, Myriam Dao, Aurélie Hummel, Bertrand Knebelman, Jean François Subra, Johan Noble, Christophe Mariat, Noémie Jourde-Chiche, Fatouma Toure, Cyril Garrouste, Charlotte Laurent, Lacraz Adeline, Yahsou Delmas, Alexandre Cez, Olivier Fritz, Christiane Mousson, Lise Marie Pouteau, Olivier Moranne, Jean-Michel Halimi, Vincent Audard
Kidney Int Rep, 2021 May, PMID: 34386662 PMCID: PMC8343786 DOI: 10.1016/j.ekir.2021.04.029
– Transition et transfert de la néphrologie pédiatrique à la néphrologie adulte : recommandations de la filière maladies rénales rares ORKiD. [Recommendations for management of patients from pediatrics unit to adult unit: Transition and transfer program].
Sandrine Lemoine, Jennifer Radenac, Véronique Baudouin, Stéphanie Belaiche, Aurélia Bertholet-Thomas, Nathalie Buebuyck, Françoise Broux, Stéphane Burtey, Gérard Champion, Marina Charbit, Pierre Cochat, Loïc De Parscau, Yahsou Delmas, Olivier Dunand, Marie Essig, Fitsum Guebre-Egziabher, Béatrice Langellier-Bellevue, Anne-Laure Leclerc, Élodie Merieau, Bruno Moulin, Justine Perrin, Dominique Rousiot, Béatrice Sartoris, Aude Servais, Arvind Nagra, Robert Novo
Nephrol Ther, 2021 Apr, PMID: 33531259 DOI: 10.1016/j.nephro.2020.10.009
– COVID-19 severity in kidney transplant recipients is similar to nontransplant patients with similar comorbidities.
Nathalie Chavarot, Juliette Gueguen, Guillaume Bonnet, Mariam Jdidou, Antonin Trimaille, Carole Burger, Lucile Amrouche, Orianne Weizman, Thibaut Pommier, Olivier Aubert, Joffrey Celier, Rebecca Sberro-Soussan, Laura Geneste, Vassili Panagides, Michel Delahousse, Wassima Marsou, Claire Aguilar, Antoine Deney, Julien Zuber, Charles Fauvel, Christophe Legendre, Delphine Mika, Theo Pezel, Dany Anglicheau, Willy Sutter, Mohamad Zaidan, Renaud Snanoudj, Ariel Cohen, Anne Scemla; Critical COVID-19 France Investigators
Am J Transplant, 2021 Mar, PMID: 33252201 PMCID: PMC7753406 DOI: 10.1111/ajt.16416
– HLA-D and PLA2R1 risk alleles associate with recurrent primary membranous nephropathy in kidney transplant recipients.
Lena Berchtold, Eric Letouzé, Mariam Priya Alexander, Guillaume Canaud, Anne-Els van de Logt, Patrick Hamilton, Christiane Mousson, Vincent Vuiblet, Ann M Moyer, Sylvain Guibert, Petra Mrázová, Charlène Levi, Valérie Dubois, Josep Maria Cruzado, Armando Torres, Manish J Gandhi, Nadhir Yousfi, Vladimir Tesar, Ondrej Viklický, Maryvonne Hourmant, Bruno Moulin, Philippe Rieu, Gabriel Choukroun, Christophe Legendre, Jack Wetzels, Paul Brenchley, José Aurelio Ballarín Castan, Hanna Debiec, Pierre Ronco
Kidney Int, 2021 Mar, PMID: 32889013 DOI: 10.1016/j.kint.2020.08.007
– The spectrum of kidney biopsies in hospitalized patients with COVID-19, acute kidney injury, and/or proteinuria.
Sophie Ferlicot, Matthieu Jamme, François Gaillard, Julie Oniszczuk, Aymeric Couturier, Olivia May, Anne Grünenwald, Aurélie Sannier, Anissa Moktefi, Ophélie Le Monnier, Camille Petit-Hoang, Nadine Maroun, Albane Brodin-Sartorius, Arthur Michon, Hélène Dobosziewicz, Fabrizio Andreelli, Matthieu Guillet, Hassane Izzedine, Christian Richard, Manon Dekeyser, Romain Arrestier, Thomas Sthelé, Edouard Lefèvre, Alexis Mathian, Christophe Legendre, Charlotte Mussini, Marie-Christine Verpont, Nicolas Pallet, Zahir Amoura, Marie Essig, Renaud Snanoudj, Isabelle Brocheriou-Spelle, Hélène François, Xavier Belenfant, Guillaume Geri, Eric Daugas, Vincent Audard, David Buob, Ziad A Massy, Mohamad Zaidan; AP-HP/Universities/Inserm COVID-19 research collaboration
Nephrol Dial Transplant, 2021 Feb 12, PMID: 33576823 PMCID: PMC7928708 DOI: 10.1093/ndt/gfab042
– Decline and loss of anti-SARS-CoV-2 antibodies in kidney transplant recipients in the 6 months following SARS-CoV-2 infection.
Nathalie Chavarot, Marianne Leruez-Ville, Anne Scemla, Carole Burger, Lucile Amrouche, Claire Rouzaud, Xavier Lebreton, Frank Martinez, Rebecca Sberro-Soussan, Christophe Legendre, Julien Zuber, Dany Anglicheau
Kidney Int, 2021 Feb, PMID: 33509358 PMCID: PMC7830266 DOI: 10.1016/j.kint.2020.12.001
– Solid organ transplantation in the era of COVID-19: Lessons from France.
Mohamad Zaidan, Christophe Legendre
Transplantation, 2021 Jan, PMID: 33208691 DOI: 10.1097/TP.0000000000003536
– Management of post-transplant recurrent focal and segmental glomerulosclerosis.
Morin G, Legendre C, Canaud G
Nephrol Dial Transplant, 2021 Nov 9, PMID: 32087022 DOI: 10.1093/ndt/gfaa021
– Study design and baseline characteristics of the CARDINAL Trial: A Phase 3 Study of Bardoxolone Methyl in Patients with Alport Syndrome.
Glenn M Chertow, Gerald B Appel, Sharon Andreoli, Sripal Bangalore, Geoffrey A Block, Arlene B Chapman, Melanie P Chin, Keisha L Gibson, Angie Goldsberry, Kazumoto Iijima, Lesley A Inker, Bertrand Knebelmann, Laura H Mariani, Colin J Meyer, Kandai Nozu, Megan O’Grady, Arnold L Silva, Peter Stenvinkel, Roser Torra, Bradley A Warady, Pablo E Pergola
Am J Nephrol, 2021, PMID: 33789284 PMCID: PMC8220919 DOI: 10.1159/000513777
2022
– Effects of Bardoxolone Methyl in Alport Syndrome.
Bradley A Warady, Pablo E Pergola, Rajiv Agarwal, Sharon Andreoli, Gerald B Appel, Sripal Bangalore, Geoffrey A Block, Arlene B Chapman, Melanie P Chin, Keisha L Gibson, Angie Goldsberry, Kazumoto Iijima, Lesley A Inker, Clifford E Kashtan, Bertrand Knebelmann, Laura H Mariani, Colin J Meyer, Kandai Nozu, Megan O’Grady, Michelle N Rheault, Arnold L Silva, Peter Stenvinkel, Roser Torra, Glenn M Chertow
Clin J Am Soc Nephrol, 2022 Dec, PMID: 36411058 PMCID: PMC9718021 DOI: 10.2215/CJN.02400222
– Absence of Mortality Differences Between the First and Second COVID-19 Waves in Kidney Transplant Recipients.
Bastien Berger, Marc Hazzan, Nassim Kamar, Hélène Francois, Marie Matignon, Clarisse Greze, Philippe Gatault, Luc Frimat, Pierre F Westeel, Valentin Goutaudier, Renaud Snanoudj, Charlotte Colosio, Antoine Sicard, Dominique Bertrand, Christiane Mousson, Jamal Bamoulid, Antoine Thierry, Dany Anglicheau, Lionel Couzi, Jonathan M Chemouny, Agnes Duveau, Valerie Moal, Yannick Le Meur, Gilles Blancho, Jérôme Tourret, Paolo Malvezzi, Christophe Mariat, Jean-Philippe Rerolle, Nicolas Bouvier, Sophie Caillard, Olivier Thaunat; French Solid Organ Transplant (SOT) COVID Registry
Kidney Int Rep, 2022 Dec, PMID: 36159445 PMCID: PMC9489985 DOI: 10.1016/j.ekir.2022.09.007
– Machine learning-supported interpretation of kidney graft elementary lesions in combination with clinical data.
Marc Labriffe, Jean-Baptiste Woillard, Wilfried Gwinner, Jan-Hinrich Braesen, Dany Anglicheau, Marion Rabant, Priyanka Koshy, Maarten Naesens, Pierre Marquet
Am J Transplant, 2022 Dec, PMID: 36062389 DOI: 10.1111/ajt.17192
– De novo posttransplant membranous nephropathy following BNT162b2 mRNA COVID-19 vaccine in a kidney transplant recipient.
Nathalie Chavarot, Michael Padden, Lucile Amrouche, Stéphanie Malard, Anne Scemla, Rebecca Sberro-Soussan, Juliette Léon, Christophe Legendre, Jean Paul Duong, Julien Zuber, Dany Anglicheau, Marion Rabant, Pierre Isnard
Am J Transplant, 2022 Dec, PMID: 35959598 PMCID: PMC9537991 DOI: 10.1111/ajt.17166
– The ABCD of Kidney Allograft Pathology-The Beginning of the Beginning.
Thangamani Muthukumar, Dany Anglicheau
J Am Soc Nephrol, 2022 Nov, PMID: 36216509 PMCID: PMC9678039 DOI: 10.1681/ASN.2022080967
– Data-Driven Chronic Allograft Phenotypes: A Novel and Validated Complement for Histologic Assessment of Kidney Transplant Biopsies.
Thibaut Vaulet, Gillian Divard, Olivier Thaunat, Priyanka Koshy, Evelyne Lerut, Aleksandar Senev, Olivier Aubert, Elisabet Van Loon, Jasper Callemeyn, Marie-Paule Emonds, Amaryllis Van Craenenbroeck, Katrien De Vusser, Ben Sprangers, Maud Rabeyrin, Valérie Dubois, Dirk Kuypers, Maarten De Vos, Alexandre Loupy, Bart De Moor, Maarten Naesens
J Am Soc Nephrol, 2022 Nov, PMID: 36316096 PMCID: PMC9678036 DOI: 10.1681/ASN.2022030290
– Atypical severe early-onset nephrotic syndrome: Answers.
Romain Berthaud, Laurence Heidet, Mehdi Oualha, Roselyne Brat, Déborah Talmud, Florentine Garaix, Marion Rabant, Véronique Frémeaux-Bacchi, Corinne Antignac, Olivia Boyer, Guillaume Dorval
Pediatr Nephrol, 2022 Nov, PMID: 35507148 DOI: 10.1007/s00467-022-05537-x
– Atypical severe early-onset nephrotic syndrome: Questions.
Romain Berthaud, Laurence Heidet, Mehdi Oualha, Roselyne Brat, Déborah Talmud, Florentine Garaix, Marion Rabant, Véronique Frémeaux-Bacchi, Corinne Antignac, Olivia Boyer, Guillaume Dorval
Pediatr Nephrol, 2022 Nov, PMID: 35507145 DOI: 10.1007/s00467-022-05521-5
– Results from a nationwide retrospective cohort measure the impact of C3 and soluble C5b-9 levels on kidney outcomes in C3 glomerulopathy.
Sophie Chauvet, Jill J Hauer, Florent Petitprez, Marion Rabant, Paula Vieira Martins, Véronique Baudouin, Yahsou Delmas, Noémie Jourde-Chiche, Alexandre Cez, David Ribes, Sylvie Cloarec, Aude Servais, Mohamad Zaidan, Eric Daugas, Michel Delahousse, Alain Wynckel, Amélie Ryckewaert, Anne Laure Sellier-Leclerc, Olivia Boyer, Eric Thervet, Alexandre Karras, Richard J H Smith, Véronique Frémeaux-Bacchi
Kidney Int, 2022 Oct, PMID: 35752323 PMCID: PMC10588728 DOI: 10.1016/j.kint.2022.05.027
– MicroRNAs in kidney injury and disease.
Nassim Mahtal, Olivia Lenoir, Claire Tinel, Dany Anglicheau, Pierre-Louis Tharaux
Nat Rev Nephrol, 2022 Oct, PMID: 35974169 DOI: 10.1038/s41581-022-00608-6
– Oral Coenzyme Q10 supplementation leads to better preservation of kidney function in steroid-resistant nephrotic syndrome due to primary Coenzyme Q10 deficiency.
Stefania Drovandi, Beata S Lipska-Ziętkiewicz, Fatih Ozaltin, Francesco Emma, Bora Gulhan, Olivia Boyer, Agnes Trautmann, Hong Xu, Qian Shen, Jia Rao, Korbinian M Riedhammer, Uwe Heemann, Julia Hoefele, Sarah L Stenton, Alexey N Tsygin, Kar-Hui Ng, Svitlana Fomina, Elisa Benetti, Manon Aurelle, Larisa Prikhodina, Michiel F Schreuder, Mansoureh Tabatabaeifar, Maciej Jankowski, Sergey Baiko, Jianhua Mao, Chunyue Feng, Cuihua Liu, Shuzhen Sun, Fang Deng, Xiaowen Wang, Stéphanie Clavé, Małgorzata Stańczyk, Irena Bałasz-Chmielewska, Marc Fila, Anne M Durkan, Tanja Kersnik Levart, Ismail Dursun, Nasrin Esfandiar, Dorothea Haas, Anna Bjerre, Ali Anarat, Marcus R Benz, Saeed Talebi, Nakysa Hooman, Gema Ariceta; PodoNet Consortium; mitoNET Consortium; CCGKDD Consortium; Franz Schaefer
Kidney Int, 2022 Sep, PMID: 35643375 DOI: 10.1016/j.kint.2022.04.029
– Variation of the clinical spectrum and genotype-phenotype associations in Coenzyme Q10 deficiency associated glomerulopathy.
Stefania Drovandi, Beata S Lipska-Ziętkiewicz, Fatih Ozaltin, Francesco Emma, Bora Gulhan, Olivia Boyer, Agnes Trautmann, Szymon Ziętkiewicz, Hong Xu, Qian Shen, Jia Rao, Korbinian M Riedhammer, Uwe Heemann, Julia Hoefele, Sarah L Stenton, Alexey N Tsygin, Kar-Hui Ng, Svitlana Fomina, Elisa Benetti, Manon Aurelle, Larisa Prikhodina, Anne M Schijvens, Mansoureh Tabatabaeifar, Maciej Jankowski, Sergey Baiko, Jianhua Mao, Chunyue Feng, Fang Deng, Caroline Rousset-Rouviere, Małgorzata Stańczyk, Irena Bałasz-Chmielewska, Marc Fila, Anne M Durkan, Tanja Kersnik Levart, Ismail Dursun, Nasrin Esfandiar, Dorothea Haas, Anna Bjerre, Ali Anarat, Marcus R Benz, Saeed Talebi, Nakysa Hooman, Gema Ariceta; PodoNet Consortium; mitoNET Consortium; CCGKDD Consortium; Franz Schaefer
Kidney Int, 2022 Sep, PMID: 35483523 DOI: 10.1016/j.kint.2022.02.040
– European Guideline for the Management of Kidney Transplant Patients With HLA Antibodies: By the European Society for Organ Transplantation Working Group.
Nizam Mamode, Oriol Bestard, Frans Claas, Lucrezia Furian, Siân Griffin, Christophe Legendre, Liset Pengel, Maarten Naesens
Transpl Int, 2022 Aug 10, PMID: 36033645 PMCID: PMC9399356 DOI: 10.3389/ti.2022.10511
– Managing immune checkpoint inhibition in transplant recipients.
Céleste Lebbé, Lucie Biard, Julie Delyon, Julien Zuber
Lancet Oncol, 2022 Aug, PMID: 35809596 DOI: 10.1016/S1470-2045(22)00395-3
– Benign and malignant proliferation in idiopathic nephrotic syndrome: a French cohort study.
Clara Cébron, Astrid Godron-Dubrasquet, Nathalie Aladjidi, Gwenaelle Roussey, Olivia Boyer, Marina Avramescu, Veronique Baudouin, Joelle Terzic, Emma Allain-Launay, Frédéric Rieux-Laucat, Stéphane Decramer, Thomas Simon, Jérôme Harambat
Pediatr Nephrol, 2022 Aug, PMID: 35006357 DOI: 10.1007/s00467-021-05386-0
– Multicentric Carpotarsal Osteolysis Syndrome Associated Nephropathy: Novel Variants of MAFB Gene and Literature Review.
Stefania Drovandi, Francesca Lugani, Olivia Boyer, Edoardo La Porta, Paolo Giordano, Aurélie Hummel, Bertrand Knebelmann, Joséphine Cornet, Genevieve Baujat, Beata S Lipska-Ziętkiewicz, Gian Marco Ghiggeri, Gianluca Caridi, Andrea Angeletti
J Clin Med, 2022 Jul 29, PMID: 35956038 PMCID: PMC9369440 DOI: 10.3390/jcm11154423
– Human C-terminal CUBN variants associate with chronic proteinuria and normal renal function.
Mathilda Bedin, Olivia Boyer, Aude Servais, Yong Li, Laure Villoing-Gaudé, Marie-Josephe Tête, Alexandra Cambier, Julien Hogan, Veronique Baudouin, Saoussen Krid, Albert Bensman, Florie Lammens, Ferielle Louillet, Bruno Ranchin, Cecile Vigneau, Iseline Bouteau, Corinne Isnard-Bagnis, Christoph J Mache, Tobias Schäfer, Lars Pape, Markus Gödel, Tobias B Huber, Marcus Benz, Günter Klaus, Matthias Hansen, Kay Latta, Olivier Gribouval, Vincent Morinière, Carole Tournant, Maik Grohmann, Elisa Kuhn, Timo Wagner, Christine Bole-Feysot, Fabienne Jabot-Hanin, Patrick Nitschké, Tarunveer S Ahluwalia, Anna Köttgen, Christian Brix Folsted Andersen, Carsten Bergmann, Corinne Antignac, Matias Simons
J Clin Invest, 2022 Jun 1, PMID: 35642643 PMCID: PMC9151686 DOI: 10.1172/JCI161852
– Early treatment with sotrovimab monoclonal antibody in kidney transplant recipients with Omicron infection.
Nathalie Chavarot, Clea Melenotte, Lucile Amrouche, Claire Rouzaud, Rebecca Sberro-Soussan, Juliette Pavie, Frank Martinez, Anne Pouvaret, Marianne Leruez-Ville, Delphine Cantin, Jacques Fourgeaud, Claire Delage, Damien Vimpere, Marie Noëlle Peraldi, Christophe Legendre, Fanny Lanternier, Julien Zuber, Anne Scemla, Dany Anglicheau
Kidney Int, 2022 Jun, PMID: 35421508 PMCID: PMC9001009 DOI: 10.1016/j.kint.2022.04.003
– Long-Term Efficacy and Safety of Repeated Rituximab to Maintain Remission in Idiopathic Childhood Nephrotic Syndrome: An International Study.
Eugene Yu-Hin Chan, Ellen L M Yu, Andrea Angeletti, Zainab Arslan, Biswanath Basu, Olivia Boyer, Chang-Yien Chan, Manuela Colucci, Guillaume Dorval, Claire Dossier, Stefania Drovandi, Gian Marco Ghiggeri, Debbie S Gipson, Riku Hamada, Julien Hogan, Kenji Ishikura, Koichi Kamei, Markus J Kemper, Alison Lap-Tak Ma, Rulan S Parekh, Seetha Radhakrishnan, Priya Saini, Qian Shen, Rajiv Sinha, Chantida Subun, Sharon Teo, Marina Vivarelli, Hazel Webb, Hong Xu, Hui Kim Yap, Kjell Tullus
J Am Soc Nephrol, 2022 Jun, PMID: 35354600 PMCID: PMC9161790 DOI: 10.1681/ASN.2021111472
– Idiopathic nephrotic syndrome relapse following COVID-19 vaccination: a series of 25 cases.
Aurélie Hummel, Julie Oniszczuk, Delphine Kervella, Marina Charbit, Dominique Guerrot, Angelo Testa, Carole Philipponnet, Cécile Chauvet, Thomas Guincestre, Karine Brochard, Ariane Benezech, Lucile Figueres, Xavier Belenfant, Andrea Guarnieri, Nathalie Demoulin, Elisa Benetti, Marius Miglinas, Kathleen Dessaix, Johann Morelle, Andrea Angeletti, Anne-Laure Sellier-Leclerc, Bruno Ranchin, Guillaume Goussard, Laurent Hudier, Justine Bacchetta, Aude Servais, Vincent Audard
Clin Kidney J, 2022 May 6, PMID: 35979142 PMCID: PMC9129143 DOI: 10.1093/ckj/sfac134
– The 2019 and 2021 International Workshops on Alport Syndrome.
Sergio Daga, Jie Ding, Constantinos Deltas, Judy Savige, Beata S Lipska-Ziętkiewicz, Julia Hoefele, Frances Flinter, Daniel P Gale, Marina Aksenova, Hirofumi Kai, Laura Perin, Moumita Barua, Roser Torra, Jeff H Miner, Laura Massella, Danica Galešić Ljubanović, Rachel Lennon, Andrè B Weinstock, Bertrand Knebelmann, Agne Cerkauskaite, Susie Gear, Oliver Gross, A Neil Turner, Margherita Baldassarri, Anna Maria Pinto, Alessandra Renieri
Eur J Hum Genet, 2022 May, PMID: 35260866 PMCID: PMC8904161 DOI: 10.1038/s41431-022-01075-0
– Long-term health-related quality of life outcomes of adults with pediatric onset of frequently relapsing or steroid-dependent nephrotic syndrome.
Marie-Sophie Meuleman, Sophie Guilmin-Crépon, Aurélie Hummel, Eric Daugas, Agnès Dumas, Fallou Leye, Jacques Dantal, Claire Rigothier, François Provot, Dominique Chauveau, Stéphane Burtey, Alexandre Hertig, Karine Dahan, Antoine Durrbach, Claire Dossier, Alexandre Karras, Dominique Guerrot, Vincent Esnault, Philippe Rémy, Ziad A Massy, Isabelle Tostivint, Marie-Pascale Morin, Philippe Zaoui, Olivier Fritz, Moglie Le Quintrec, Alain Wynckel, Aurélie Bourmaud, Olivia Boyer, Dil Sahali, Corinne Alberti, Vincent Audard, Hélène Mellerio
J Nephrol, 2022 May, PMID: 34224090 DOI: 10.1007/s40620-021-01111-0
– The MHC class I MICA gene is a histocompatibility antigen in kidney transplantation.
Raphael Carapito, Ismail Aouadi, Martin Verniquet, Meiggie Untrau, Angélique Pichot, Thomas Beaudrey, Xavier Bassand, Sébastien Meyer, Loic Faucher, Juliane Posson, Aurore Morlon, Irina Kotova, Florent Delbos, Alexandre Walencik, Alice Aarnink, Anne Kennel, Caroline Suberbielle, Jean-Luc Taupin, Benedict M Matern, Eric Spierings, Nicolas Congy-Jolivet, Arnaud Essaydi, Peggy Perrin, Antoine Blancher, Dominique Charron, Nezih Cereb, Myriam Maumy-Bertrand, Frédéric Bertrand, Valérie Garrigue, Vincent Pernin, Laurent Weekers, Maarten Naesens, Nassim Kamar, Christophe Legendre, Denis Glotz, Sophie Caillard, Marc Ladrière, Magali Giral, Dany Anglicheau, Caner Süsal, Seiamak Bahram
Nat Med, 2022 May, PMID: 35288692 PMCID: PMC9117142 DOI: 10.1038/s41591-022-01725-2
– New Equations for Estimating the GFR without Race.
Marc Raynaud, Olivier Aubert, Alexandre Loupy
N Engl J Med, 2022 Apr 28, PMID: 35476657 DOI: 10.1056/NEJMc2119761
– Long-term survival benefit from dual kidney transplantation using kidneys from donors with very extended criteria-a French cohort between 2002 and 2014.
Emilie Savoye, Christophe Legendre, Yann Neuzillet, Marie-Noëlle Peraldi, Philippe Grimbert, Nacera Ouali, Matthieu Durand, Lionel Badet, François Kerbaul, Myriam Pastural, Camille Legeai, Marie-Alice Macher, Renaud Snanoudj
Nephrol Dial Transplant, 2022 Apr 25, PMID: 34748014 DOI: 10.1093/ndt/gfab317
– The genetics of steroid-resistant nephrotic syndrome in children.
Guillaume Dorval, Aude Servais, Olivia Boyer
Nephrol Dial Transplant, 2022 Mar 25, PMID: 33180925 DOI: 10.1093/ndt/gfaa221
– Kidney transplantation from expanded criteria donors: an increased risk of urinary complications – the UriNary Complications Of Renal Transplant (UNyCORT) study.
Benoit Mesnard, Maxime Leroy, James Hunter, Delphine Kervella, Marc-Olivier Timsit, Lionel Badet, Pascal Glemain, Emmanuel Morelon, Fanny Buron, Moglie Le Quintrec-Donnette, Vincent Pernin, Marc Ladriere, Sophie Girerd, Christophe Legendre, Antoine Sicard, Laeticia Albano, Stephane De Vergie, Clarisse Kerleau, Thomas Prudhomme, Jérôme Rigaud, Diego Cantarovich, Gilles Blancho, Georges Karam, Magali Giral, Simon Ville, Julien Branchereau; Données Informatisées et VAlidées en Transplantation/Computerized and VAlidated Data in Transplantation (DIVAT) Consortium Affiliations
BJU Int, 2022 Feb, PMID: 34114727 DOI: 10.1111/bju.15509
2023
– The spectrum of glomerular and vascular kidney pathology associated with myeloproliferative neoplasms.
Thibaut d’Izarny-Gargas, Pierre Isnard, Idris Boudhabhay, David Buob, Anissa Moktefi, Charel Linster, Aurélie Hummel, Emmanuel Esteve, Vincent Audard, Hélène Lazareth, Nadine Maroun, Alexandre Hertig, Clément Gosset, Charlotte Jouzel, Sarah Permal, Camille Domenger, Olivier Kosmider, Marion Rabant, Alexandre Karras, Jean-Paul Duong Van Huyen
Kidney Int, 2023 Dec, PMID: 37769965 DOI: 10.1016/j.kint.2023.09.010
– A Validated LC-MS/MS Method for Performing Belatacept Drug Monitoring in Renal Transplantation.
Stéphanie Chhun, Mathieu Trauchessec, Sophie Melicine, Frédéric Nicolas, Agathe Miele, Srboljub Lukic, Estelle Vilain, Lucile Amrouche, Dorothée Lebert, Dany Anglicheau, Eric Tartour, Julien Zuber
Biomedicines, 2023 Nov 1, PMID: 38001955 PMCID: PMC10669563 DOI: 10.3390/biomedicines11112955
– Rare Variants in Complement Gene in C3 Glomerulopathy and Immunoglobulin-Mediated Membranoproliferative GN.
Marie Sophie Meuleman, Paula Vieira-Martins, Carine El Sissy, Vincent Audard, Véronique Baudouin, Dominique Bertrand, Frank Bridoux, Férielle Louillet, Claire Dossier, Vincent Esnault, Noémie Jourde-Chiche, Alexandre Karras, Marie-Pascale Morin, François Provot, Philippe Remy, David Ribes, Caroline Rousset-Rouviere, Aude Servais, Eric Thervet, Leila Tricot, Mohamad Zaidan, Alain Wynckel, Julien Zuber, Moglie Le Quintrec, Véronique Frémeaux-Bacchi, Sophie Chauvet
Clin J Am Soc Nephrol, 2023 Nov 1, PMID: 37615951 PMCID: PMC10637453 DOI: 10.2215/CJN.0000000000000252
– Targeting the Complement Pathway in Kidney Transplantation.
Dela Golshayan, Nora Schwotzer, Fadi Fakhouri, Julien Zuber
J Am Soc Nephrol, 2023 Nov 1, PMID: 37439664 PMCID: PMC10631604 DOI: 10.1681/ASN.0000000000000192
– Vaccination practices in pediatric transplantation: A survey among member centers of the European reference network TransplantChild.
Daniele Donà, Luz Yadira Bravo-Gallego, Esteban Frauca Remacha, Mara Cananzi, Andrea Gastaldi, Juan Torres Canizalez, Xavier Stephenne, Florence Lacaille, Caroline Lindemans, Elisabetta Calore, Nathalie Galea, Elisa Benetti, Edith Nachbaur, Ana Rita Sandes, Ana Teixeira, Sandra Ferreira, Maja Klaudel-Dreszler, Oanez Ackermann, Olivia Boyer, Laura Espinosa, Luis García Guereta, Marco Sciveres, Björn Fischler, Nicolaus Schwerk, Mette Neland, Emanuele Nicastro, Luca Dello Strologo, Jacek Toporski, Inga Vainumae, Jelena Rascon, Vaidotas Urbonas, Teresa Del Rosal, Eduardo López-Granados, Giorgio Perilongo, Alastair Baker, Paloma Jara Vega; ERN TransplantChild Healthcare Working Group
Pediatr Transplant, 2023 Nov, PMID: 37543721 DOI: 10.1111/petr.14589
– Validation of a prediction system for risk of kidney allograft failure in pediatric kidney transplant recipients: An international observational study.
Julien Hogan, Gillian Divard, Olivier Aubert, Rouba Garro, Olivia Boyer, Lee Alex Donald Cooper, Alton Brad Farris, Marc Fila, Michael Seifert, Anne-Laure Sellier-Leclerc, Jody Smith, Alexander Fichtner, Burkhard Tönshoff, Katherine Twombley, Bradley Warady, Meghan Pearl, Rima S Zahr, Carmen Lefaucheur, Rachel Patzer, Alexandre Loupy
Am J Transplant, 2023 Oct, PMID: 37453485 PMCID: PMC11247401 DOI: 10.1016/j.ajt.2023.07.004
– Childhood nephrotic syndrome.
Marina Vivarelli, Keisha Gibson, Aditi Sinha, Olivia Boyer
Lancet, 2023 Sep 2, PMID: 37659779 DOI: 10.1016/S0140-6736(23)01051-6
– Rituximab-associated hypogammaglobulinemia in children with idiopathic nephrotic syndrome: results of an ESPN survey.
Aleksandra Zurowska, Magdalena Drozynska-Duklas, Rezan Topaloglu, Antonia Bouts, Olivia Boyer, Mohan Shenoy, Marina Vivarelli; ESPN Glomerulonephritis Working Group
Pediatr Nephrol, 2023 Sep, PMID: 37014530 PMCID: PMC10432325 DOI: 10.1007/s00467-023-05913-1
– Renal vein thrombosis in neonates: a case series of diagnosis, treatment and childhood kidney function follow-up.
Bellaure Ndoudi Likoho, Romain Berthaud, Claire Dossier, Jean-Daniel Delbet, Olivia Boyer, Véronique Baudouin, Marianne Alison, Valérie Biran, Marie-Françoise Hurtaud, Julien Hogan, Theresa Kwon, Anne Couderc
Pediatr Nephrol, 2023 Sep, PMID: 36988695 DOI: 10.1007/s00467-023-05918-w
– Immunogenicity of Anti-SARS-CoV-2 Vaccination After Kidney Transplantation in Kidney Transplant Recipients Vaccinated Before Transplantation.
Charlotte Uro-Coste, Rebecca Sberro-Soussan, Frank Martinez, Lucile Amrouche, Olivier Aubert, Marianne Leruez-Ville, Claire Delage, Marie Noëlle Peraldi, Christophe Legendre, Fanny Lanternier, Julien Zuber, Dany Anglicheau, Anne Scemla, Nathalie Chavarot
Transplantation, 2023 Aug 1, PMID: 37211632 PMCID: PMC10358298 DOI: 10.1097/TP.0000000000004654
– Transcriptional and spatial profiling of the kidney allograft unravels a central role for FcyRIII+ innate immune cells in rejection.
Baptiste Lamarthée, Jasper Callemeyn, Yannick Van Herck, Asier Antoranz, Dany Anglicheau, Patrick Boada, Jan Ulrich Becker, Tim Debyser, Frederik De Smet, Katrien De Vusser, Maëva Eloudzeri, Amelie Franken, Wilfried Gwinner, Priyanka Koshy, Dirk Kuypers, Diether Lambrechts, Pierre Marquet, Virginie Mathias, Marion Rabant, Minnie M Sarwal, Aleksandar Senev, Tara K Sigdel, Ben Sprangers, Olivier Thaunat, Claire Tinel, Thomas Van Brussel, Amaryllis Van Craenenbroeck, Elisabet Van Loon, Thibaut Vaulet, Francesca Bosisio, Maarten Naesens
Nat Commun, 2023 Jul 19, PMID: 37468466 PMCID: PMC10356785 DOI: 10.1038/s41467-023-39859-7
– Race-free estimated glomerular filtration rate equation in kidney transplant recipients: development and validation study.
Marc Raynaud, Solaf Al-Awadhi, Ivana Juric, Gillian Divard, Yannis Lombardi, Nikolina Basic-Jukic, Olivier Aubert, Laurence Dubourg, Ingrid Masson, Christophe Mariat, Dominique Prié, Vincent Pernin, Moglie Le Quintrec, Timothy S Larson, Mark D Stegall, Boris Bikbov, Piero Ruggenenti, Laurent Mesnard, Hassan N Ibrahim, Marie Bodilsen Nielsen, Arthur J Matas, Brian J Nankivell, Stan Benjamens, Robert A Pol, Stephan J L Bakker, Xavier Jouven, Christophe Legendre, Nassim Kamar, Byron H Smith, Hani M Wadei, Antoine Durrbach, Flavio Vincenti, Giuseppe Remuzzi, Carmen Lefaucheur, Andrew J Bentall, Alexandre Loupy
BMJ, 2023 May 31, PMID: 37257905 PMCID: PMC10231444 DOI: 10.1136/bmj-2022-073654
– Steroid-sensitive nephrotic syndrome in children.
Olivia Boyer, Agnes Trautmann, Dieter Haffner, Marina Vivarelli
Nephrol Dial Transplant, 2023 May 4, PMID: 36455815 DOI: 10.1093/ndt/gfac314
– An automated histological classification system for precision diagnostics of kidney allografts.
Daniel Yoo, Valentin Goutaudier, Gillian Divard, Juliette Gueguen, Brad C Astor, Olivier Aubert, Marc Raynaud, Zeynep Demir, Julien Hogan, Patricia Weng, Jodi Smith, Rouba Garro, Bradley A Warady, Rima S Zahr, Marta Sablik, Katherine Twombley, Lionel Couzi, Thierry Berney, Olivia Boyer, Jean-Paul Duong-Van-Huyen, Magali Giral, Alaa Alsadi, Pierre A Gourraud, Emmanuel Morelon, Moglie Le Quintrec, Sophie Brouard, Christophe Legendre, Dany Anglicheau, Jean Villard, Weixiong Zhong, Nassim Kamar, Oriol Bestard, Arjang Djamali, Klemens Budde, Mark Haas, Carmen Lefaucheur, Marion Rabant, Alexandre Loupy
Nat Med, 2023 May, PMID: 37142762 DOI: 10.1038/s41591-023-02323-6
– Machine learning does not outperform traditional statistical modelling for kidney allograft failure prediction.
Agathe Truchot, Marc Raynaud, Nassim Kamar, Maarten Naesens, Christophe Legendre, Michel Delahousse, Olivier Thaunat, Matthias Buchler, Marta Crespo, Kamilla Linhares, Babak J Orandi, Enver Akalin, Gervacio Soler Pujol, Helio Tedesco Silva Jr, Gaurav Gupta, Dorry L Segev, Xavier Jouven, Andrew J Bentall, Mark D Stegall, Carmen Lefaucheur, Olivier Aubert, Alexandre Loupy
Kidney Int, 2023 May, PMID: 36572246 DOI: 10.1016/j.kint.2022.12.011
– Prednisolone pharmacokinetics after oral prednisone administration in paediatric patients with kidney transplant.
Camille de Truchis, Naïm Bouazza, Frantz Foissac, Marina Charbit, Laurène Dehoux, Gabrielle Lui, Mégane Ribot, Nelly Briand, Yi Zheng, Jean-Marc Tréluyer, Olivia Boyer
Br J Clin Pharmacol, 2023 May, PMID: 36510685 DOI: 10.1111/bcp.15610
– A multicenter retrospective study of calcineurin inhibitors in nephrotic syndrome secondary to podocyte gene variants.
Georgia Malakasioti, Daniela Iancu, Anastasiia Milovanova, Alexey Tsygin, Tomoko Horinouchi, China Nagano, Kandai Nozu, Koichi Kamei, Shuichiro Fujinaga, Kazumoto Iijima, Rajiv Sinha, Biswanath Basu, William Morello, Giovanni Montini, Aoife Waters, Olivia Boyer, Zeynep Yürük Yıldırım, Sibel Yel, İsmail Dursun, Hugh J McCarthy, Marina Vivarelli, Larisa Prikhodina, Martine T P Besouw, Eugene Yu-Hin Chan, Wenyan Huang, Markus J Kemper, Sebastian Loos, Chanel Prestidge, William Wong, Galia Zlatanova, Rasmus Ehren, Lutz T Weber, Hassib Chehade, Nakysa Hooman, Marcin Tkaczyk, Małgorzata Stańczyk, Michael Miligkos, Kjell Tullus ; CNI in Monogenic SRNS Study Investigators
Kidney Int, 2023 May, PMID: 36898413 DOI: 10.1016/j.kint.2023.02.022
– Inaxaplin for Proteinuric Kidney Disease in Persons with Two APOL1 Variants.
Ogo Egbuna, Brandon Zimmerman, George Manos, Anne Fortier, Madalina C Chirieac, Leslie A Dakin, David J Friedman, Kate Bramham, Kirk Campbell, Bertrand Knebelmann, Laura Barisoni, Ronald J Falk, Debbie S Gipson, Michael S Lipkowitz, Akinlolu Ojo, Mark E Bunnage, Martin R Pollak, David Altshuler, Glenn M Chertow; VX19-147-101 Study Group
N Engl J Med, 2023 Mar 16, PMID: 36920755 DOI: 10.1056/NEJMoa2202396
– A specific molecular signature in SARS-CoV-2-infected kidney biopsies.
Pierre Isnard, Paul Vergnaud, Serge Garbay, Matthieu Jamme, Maeva Eloudzeri, Alexandre Karras, Dany Anglicheau, Valérie Galantine, Arwa Jalal Eddine, Clément Gosset, Franck Pourcine, Mohammed Zarhrate, Jean-Baptiste Gibier, Elena Rensen, Stefano Pietropaoli, Giovanna Barba-Spaeth, Jean-Paul Duong-Van-Huyen, Thierry J Molina, Florian Mueller, Christophe Zimmer, Marco Pontoglio, Fabiola Terzi, Marion Rabant
JCI Insight, 2023 Mar 8, PMID: 36749641 PMCID: PMC10077488 DOI: 10.1172/jci.insight.165192
– IPNA clinical practice recommendations for the diagnosis and management of children with steroid-sensitive nephrotic syndrome.
Agnes Trautmann, Olivia Boyer, Elisabeth Hodson, Arvind Bagga, Debbie S Gipson, Susan Samuel, Jack Wetzels, Khalid Alhasan, Sushmita Banerjee, Rajendra Bhimma, Melvin Bonilla-Felix, Francisco Cano, Martin Christian, Deirdre Hahn, Hee Gyung Kang, Koichi Nakanishi, Hesham Safouh, Howard Trachtman, Hong Xu, Wendy Cook, Marina Vivarelli, Dieter Haffner; International Pediatric Nephrology Association
Pediatr Nephrol, 2023 Mar, PMID: 36269406 PMCID: PMC9589698 DOI: 10.1007/s00467-022-05739-3
– French practical guidelines for the diagnosis and management of AA amyloidosis.
S Georgin-Lavialle, L Savey, D Buob, J-P Bastard, S Fellahi, A Karras, J-J Boffa, G Grateau; Collaborators: Vincent Audard, Franck Bridoux, R Damade, Samuel Deshayes, Irina Giurgea, Brigitte Granel, Eric Hachulla, Arnaud Hot, Arnaud Jaccard, Bertrand Knebelmann, Sebastian Marciano, Françoise Pelcot, Guillaume Sarrabay, Guilaine Boursier, Jérémie Sellam, Alexandre Terre, Rim Bourguiba
Rev Med Interne, 2023 Feb, PMID: 36759076 DOI: 10.1016/j.revmed.2022.12.004
– Bi-allelic pathogenic variants in ITGA8 cause slowly progressive renal disease of unknown etiology.
Sara Gómez-Conde, Olivier Dunand, Aurélie Hummel, Vincent Morinière, Marion Gauthier, Laurent Mesnard, Laurence Heidet
Clin Genet, 2023 Jan, PMID: 36089563 DOI: 10.1111/cge.14229
– Human kidney-derived hematopoietic stem cells can support long-term multilineage hematopoiesis.
Steicy Sobrino, Chrystelle Abdo, Bénédicte Neven, Adeline Denis, Nathalie Gouge-Biebuyck, Emmanuel Clave, Soëli Charbonnier, Tifanie Blein, Camille Kergaravat, Marion Alcantara, Patrick Villarese, Romain Berthaud, Laurène Dehoux, Souha Albinni, Esma Karkeni, Chantal Lagresle-Peyrou, Marina Cavazzana, Rémi Salomon, Isabelle André, Antoine Toubert, Vahid Asnafi, Capucine Picard, Stéphane Blanche, Elizabeth Macintyre, Olivia Boyer, Emmanuelle Six, Julien Zuber
Kidney Int, 2023 Jan, PMID: 36108807 DOI: 10.1016/j.kint.2022.08.024
2024
– Childhood idiopathic nephrotic syndrome: recent advancements shaping future guidelines.
Eugene Yu-Hin Chan, Olivia Boyer
Pediatr Nephrol, 2024 Dec 26, PMID: 39724419 DOI: 10.1007/s00467-024-06634-9
– An international, multi-center study evaluated rituximab therapy in childhood steroid-resistant nephrotic syndrome.
Eugene Yu-Hin Chan, Aditi Sinha, Ellen L M Yu, Naureen Akhtar, Andrea Angeletti, Arvind Bagga, Sushmita Banerjee, Olivia Boyer, Chang-Yien Chan, Anna Francis, Gian Marco Ghiggeri, Riku Hamada, Pankaj Hari, Nakysa Hooman, Luke Sydney Hopf, Mohamad Ikram I, Iftikhar Ijaz, Dmytro D Ivanov, Suprita Kalra, Hee Gyung Kang, Laura Lucchetti, Francesca Lugani, Alison Lap-Tak Ma, William Morello, María Dolores Camargo Muñiz, Subal Kumar Pradhan, Larisa Prikhodina, Reem H Raafat, Rajiv Sinha, Sharon Teo, Kouki Tomari, Marina Vivarelli, Hazel Webb, Hui Kim Yap, Desmond Yat-Hin Yap, Kjell Tullus
Kidney Int, 2024 Dec, PMID: 39395629 DOI: 10.1016/j.kint.2024.09.011
– B-cell repertoire and functions in idiopathic nephrotic syndrome: what to learn from single-cell RNA sequencing?
Guillaume Dorval, Manuela Colucci, Olivia Boyer
Kidney Int, 2024 Oct, PMID: 38977075 DOI: 10.1016/j.kint.2024.05.032
– Less or later: Treatment dilemmas in congenital nephrotic syndrome.
Detlef Bockenhauer, Olivia Boyer
Acta Paediatr, 2024 Aug, PMID: 38807540 DOI: 10.1111/apa.17310
– Levamisole in childhood idiopathic nephrotic syndrome: new promises, and advocacy for global access.
Eugene Yu-Hin Chan, Olivia Boyer
Kidney Int, 2024 May, PMID: 38642993 DOI: 10.1016/j.kint.2024.01.030
– Steroid-Resistant Nephrotic Syndrome due to NPHS2 Variants Is Not Associated With Posttransplant Recurrence.
Jessica Kachmar, Olivia Boyer, Beata Lipska-Ziętkiewicz, Vincent Morinière, Olivier Gribouval, Laurence Heidet, Irena Balasz-Chmielewska, Elisa Benetti, Sylvie Cloarec, Dagmar Csaicsich, Stéphane Decramer, Jutta Gellermann, Vincent Guigonis, Julien Hogan, Aysun Karabay Bayazit, Anette Melk, Nazym Nigmatullina, Jun Oh, Fatih Ozaltin, Bruno Ranchin, Michel Tsimaratos, Agnes Trautmann, Corinne Antignac, Franz Schaefer, Guillaume Dorval; PodoNet Network
Kidney Int Rep, 2024 Jan 10, PMID: 38765578 PMCID: PMC11101709 DOI: 10.1016/j.ekir.2024.01.005
– Multipopulation genome-wide association meta-analysis in pediatric steroid-sensitive nephrotic syndrome.
Olivia Boyer, Guillaume Dorval
Kidney Int, 2024 Jan, PMID: 37714428 DOI: 10.1016/j.kint.2023.08.022
– To biopsy or not to biopsy a teenager with typical idiopathic nephrotic syndrome? Start steroids first.
Olivia Boyer, Silvia Bernardi, Evgenia Preka
Pediatr Nephrol, 2024 Sep, PMID: 39259322 DOI: 10.1007/s00467-024-06447-w
2025
– A « Trial within a Cohort » platform for pediatric clinical trials on idiopathic nephrotic syndrome: scope, objectives, and design of the retrospective-prospective cohort PIN’SNP.
Claire Bahans, Olivia Boyer, Olivier Dunand, Cyrielle Parmentier, Bruno Ranchin, Gwenaëlle Roussey, Charlotte Samaille, Stéphanie Tellier, Isabelle Vrillon, Evgenia Preka, Théo Mériguet, Astrid Dubrasquet, Lydia Ichay, Stéphanie Clavé, Julie Bernardor, Elodie Merieau, Claire Dossier, Vincent Guigonis
Pediatr Nephrol, 2025 Jul, PMID: 40032676 PMCID: PMC12117012 DOI: 10.1007/s00467-025-06676-7
– Publisher Correction: Rituximab-associated hypogammaglobulinemia in children with idiopathic nephrotic syndrome: results of an ESPN survey.
Aleksandra Zurowska, Magdalena Drozynska-Duklas, Rezan Topaloglu, Antonia Bouts, Olivia Boyer, Mohan Shenoy, Marina Vivarelli; ESPN Glomerulonephritis Working Group
Pediatr Nephrol, 2025 Mar, PMID: 39699592 PMCID: PMC11753299 DOI: 10.1007/s00467-024-06625-w
– IPNA consensus definitions for clinical trial outcomes in steroid-resistant nephrotic syndrome.
Pankaj Hari, Priyanka Khandelwal, Olivia Boyer, Rajendra Bhimma, Francesco Cano, Martin Christian, Ali Duzova, Kazumoto Iijima, Hee Gyung Kang, Shen Qian, Hesham Safouh, Susan Samuels, William E Smoyer, Marina Vivarelli, Arvind Bagga, Franz Schaefer; IPNA Best Practices and Standards Committee and c4c Pediatric Nephrology Expert Working Group
Pediatr Nephrol, 2025 Mar, PMID: 39384644 DOI: 10.1007/s00467-024-06543-x
– Safety and Efficacy of Oral Direct Factor Xa Inhibitors in Patients With Nephrotic Syndrome: Results From a National Retrospective Study.
Caroline Arches, Arwa Jalal-Eddine, Dimitri Titeca-Beauport, Myriam Dao, Thierry Lobbedez, Philippe Zaoui, Christophe Masset, Dominique Bertrand, Khalil El Karoui, Henri Brenier, Hamza Sakhi, Bastien Peiffer, Vincent Audard, Nizar Joher
Kidney Int Rep, 2025 Feb 3, PMID: 40303208 PMCID: PMC12034858 DOI: 10.1016/j.ekir.2025.01.042
– Steroid pulse therapy in idiopathic nephrotic syndrome in the era of modern immunosuppressive treatment-still up to date?
Cyrielle Parmentier, Solene Victor, Claire Dossier, Jean Daniel Delbet, Julien Hogan, Antoine Mouche, Olivia Boyer, Tim Ulinski
Pediatr Nephrol, 2025 Feb, PMID: 39316153 DOI: 10.1007/s00467-024-06535-x
– To biopsy or not to biopsy a teenager with typical idiopathic nephrotic syndrome? Start steroids first.
Olivia Boyer, Silvia Bernardi, Evgenia Preka
Pediatr Nephrol, 2025 Feb, PMID: 39259322 DOI: 10.1007/s00467-024-06447-w
Pediatric nephrology
- Clinical and genetic heterogeneity in familial steroid-sensitive nephrotic syndrome.
Dorval G, Gribouval O, Martinez-Barquero V, Machuca E, Tête MJ, Baudouin V, Ronco P, Rondeau E, Sallee M, Tsimaratos M, Ulinski T, Salomon R, Antignac C, Boyer O.
Pediatr Nephrol. 2017 Oct 23. doi:10.1007/s00467-017-3819-9. [Epub ahead of print] PubMed PMID: 29058154. - A randomized clinical trial indicates that levamisole increases the time to relapse in children with steroid-sensitive idiopathic nephrotic syndrome.
Gruppen MP, Bouts AH, Jansen-van der Weide MC, (…) Niaudet P, Cornelissen EAM, Schurmans T, Raes A, van de Walle J, van Dyck M, Gulati A, Bagga A, Davin JC; all members of the Levamisole Study Group.
Kidney Int. 2017 Oct 17. pii: S0085-2538(17)30607-5. doi:10.1016/j.kint.2017.08.011. [Epub ahead of print] PubMed PMID: 29054532. - Hereditary Podocytopathies in Adults: The Next Generation.
Boyer O, Dorval G, Servais A.
Kidney Dis (Basel). 2017 Jul;3(2):50-56. doi: 10.1159/000477243. Epub 2017 May 31. Review. PubMed PMID: 28868292; PubMed Central PMCID: PMC5566765. - Epidemiology of idiopathic nephrotic syndrome in children: endemic or epidemic?
Dossier C, Lapidus N, Bayer F, Sellier-Leclerc AL, Boyer O, de Pontual L, May A, Nathanson S, Orzechowski C, Simon T, Carrat F, Deschênes G.
Pediatr Nephrol. 2016 Dec;31(12):2299-2308. Epub 2016 Oct 24. PubMed PMID:27778092.
Adult nephrology
- Roles of APOL1 G1 and G2 variants in sickle cell disease patients: kidney is the main target
Kormann R, Jannot AS, Narjoz C, Ribeil JA, Manceau S, Delville M, Joste V, Prié D, Pouchot J, Thervet E, Courbebaisse M, Arlet JB.
Br J Haematol. 2017 Oct, PMID: 28699644 DOI: 10.1111/bjh.14842 - Rituximab for Recurrence of Primary Focal Segmental Glomerulosclerosis After Kidney Transplantation: Clinical Outcomes.
Garrouste C, Canaud G, Büchler M, Rivalan J, Colosio C, Martinez F, Aniort J, Dudreuilh C, Pereira B, Caillard S, Philipponnet C, Anglicheau D, Heng AE.
Transplantation. 2017 Mar, PMID: 27043407 DOI: 10.1097/TP.0000000000001160 - Rituximab for Severe Membranous Nephropathy: A 6-Month Trial with Extended Follow-Up.
Dahan K, Debiec H, Plaisier E, Cachanado M, Rousseau A, Wakselman L, Michel PA, Mihout F, Dussol B, Matignon M, Mousson C, Simon T, Ronco P; GEMRITUX Study Group.
J Am Soc Nephrol. 2017 Jan, PMID: 27352623 PMCID: PMC5198292 DOI: 10.1681/ASN.2016040449 - The costimulatory receptor B7-1 is not induced in injured podocytes.
Baye E, Gallazzini M, Delville M, Legendre C, Terzi F, Canaud G.
Kidney Int. 2016 Nov, PMID: 27528551 PMCID: PMC5073075 DOI: 10.1016/j.kint.2016.06.022 - B7-1 Blockade Does Not Improve Post-Transplant Nephrotic Syndrome Caused by Recurrent FSGS.
Delville M, Baye E, Durrbach A, Audard V, Kofman T, Braun L, Olagne J, Nguyen C, Deschênes G, Moulin B, Delahousse M, Kesler-Roussey G, Beaudreuil S, Martinez F, Rabant M, Grimbert P, Gallazzini M, Terzi F, Legendre C, Canaud G.
J Am Soc Nephrol. 2016 Aug, PMID: 26701979 PMCID: PMC4978058 DOI: 10.1681/ASN.2015091002
Corticotherapy
Corticosteroid treatment in the form of prednisone or prednisolone for example. Corticosteroids are normally produced by the body and regulate many functions. Corticosteroids can also be given as medication because they decrease inflammation and certain immune system responses.
Diuretics
Drugs that increase the elimination of salt in the urine and consequently increase the volume of urine.
Edema
Swelling related to an excess of water and salt, often localized at the ankles or eyelids.
Idiopathic
Whose cause and mechanism is unknown.
Kidney biopsy or needle kidney biopsy
Removal of a small kidney fragment for microscopic examination.
Minimal glomerular lesions
The kidney appears normal under the microscope. This is the most common case during steroid-sensitive nephrotic syndrome.
Nephrotic syndrome
Presence of significant amounts of protein in the urine associated with a decrease in the level of albumin in the blood.
Peritonitis
Bacterial infection of the peritoneum, the membrane that surrounds the organs in the abdomen.
Remission
Disappearance of proteinuria.
Segmental or focal hyalinosis
The kidney appears under the microscope with small areas of fibrosis.
Thrombosis
Formation of a clot in a vessel whether a vein or an artery. This clot can move in a vein and migrate into the lung, causing a pulmonary embolism.
Contact information
Necker-Enfants malades university hospital
> Nephrology department
149 rue de Sèvres
75743 PARIS Cedex 15
In Necker, the reference center for idiopathic nephrotic syndrome in children and adults in brief …
* data valid for 2022